The coronavirus pandemic is a global issue that’s impacting nearly every individual and industry in different ways, but it’s been particularly trying for those in the business of saving lives. In the U.S., more than 300,000 people and counting have died from complications associated with COVID-19.
“Healthcare workers have become the frontline battling the pandemic, as if it were in a faraway land and something you only see on TV,” says Phil Franks (’08), a retired U.S. Army Medical Service Corps officer and helicopter pilot. Previously the director of system operations for the Los Angeles County Department of Health Services (DHS), Franks was recently named system CEO for two new Signature Healthcare hospitals in Orange County, California.
“There are so many things only seen and heard in the hospital … society doesn’t understand what’s asked of you,” he says.
At the same time, the crisis sparks a heightened sense of purpose, energy and drive to serve, he adds. “You are anxious, scared, and paradoxically, excited to tackle the challenge.”
For Franks and two other Embry-Riddle alumni who are healthcare leaders, COVID-19 is at once the challenge of their careers and the opportunity to effect meaningful change for their hospitals and communities.
“Going through this has forced us, like most healthcare organizations, to rethink how we deliver care,” says Dr. Dan Handel (’10), vice president and chief medical officer at Indiana University (IU) Health – South Central Region.
A practicing physician at four emergency departments in the IU Health system, Handel says the coronavirus prompted a level of operational nimbleness that didn’t exist before. When COVID-19 cases amplified in March, hospitals stopped offering elective surgeries to ensure patient safety and profits tumbled, he says.
The IU Health system rallied after the first peak of COVID-19, implementing measures that allowed critical care of coronavirus-infected patients and elective surgical procedures to take place in tandem. When a second, even greater spike of coronavirus-infected patients flooded the hospital system in July, Handel says, they were ready. “We’re now operating in an environment where we can serve both needs.”
Telemedicine Advancements
Another positive development at IU Health is the growth of telemedicine — where doctors meet with patients over the phone or via an online face-to-face platform.
“Telehealth is now being hardwired into a part of how we deliver care, which opens up all sorts of possibilities in access to care, especially for our rural and underserved populations who may have transportation issues,” he says.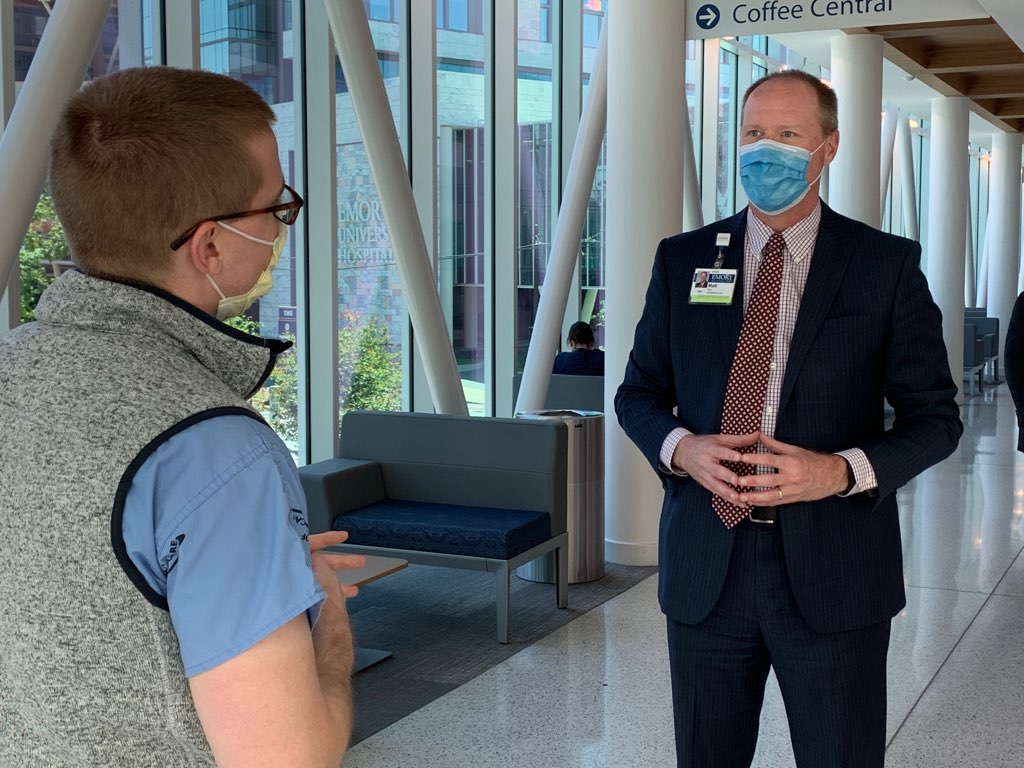
Matt Wain (’95), the CEO of Emory University Hospital and two other hospitals in the Emory Healthcare system in Atlanta, sees this benefit, as well. “We’re now doing 15,000 telemedicine visits a week; we were doing a fraction before,” Wain says.
The virus has also spurred drug advancements, including clinical trials on antiviral medications, like Remdesivir, which was trialed as an experimental treatment for Ebola during the 2014 outbreak in West Africa. Trials of Remdesivir are showing favorable results for those infected with COVID-19, Wain says.
“Our ability to continue innovative therapeutics — in this case more patients were enrolled in the Remdesivir trial (ACTT-1) at Emory than anywhere else in the world — contributed significantly to the drug’s approval and national success story,” he says.
Flexing Operational Muscle
Wain also championed innovations in hospital operations to deal with COVID-19. “We created and honed ‘warm zones’ and ultraviolet reprocessing of personal protective equipment (PPE),” he says. Instead of “donning and doffing” facemasks and other PPE before and after each patient visit, staff working in designated COVID-19 areas, or warm zones, would wear the same PPE from room to room. “The key here,” Wain says, “is that this is done while PPE is in good shape.” This practice helped conserve the hospitals’ PPE supplies during peaks in demand while simplifying the patient care workflow for providers.
“Healthcare workers have become the frontline battling the pandemic, as if it were in a faraway land and something you only see on TV … society doesn’t understand what’s asked of you.”
“The warm zones were a game change, such that we could still protect people,” he says. The hospitals implemented stringent COVID-19 testing of their employees, demonstrating the practice was safe. “It was an evidence-based approach to the problem,” Wain says.
Wain, who retired from the U.S. Army Reserve in 2008, credits his staff for the hospitals’ successes. “At the end of the day, we win or lose with our people. As a leader, it’s an honor to shepherd a culture that has risen to the challenge of our generations.”
A Disruptive Force
As the chief operations officer for the nation’s second largest municipal health system and the largest county-run correctional health system when the pandemic hit LA, Franks says the coronavirus was and is disruptive. “COVID has challenged every facet of our healthcare system; there’s nothing it hasn’t touched in some way.”
While bed space, PPE and ventilators were top supply concerns, respiratory staffing was an unanticipated challenge, he says.
The hospital transfer infrastructure that Franks established in 2018 for LA County DHS was instrumental in helping find solutions for staffing and care demands. The patient-flow management system was originally designed to get patients who presented at out-of-network hospitals back to their “home” hospital (or repatriated) to the LA County healthcare system. When the pandemic hit California in March, Franks reverse-engineered the transfer center’s operations to protect non-COVID-19 patients and focus critical care resources where the need was greatest.
Patients were sent to locations like the newly formed LA Surge Hospital, USNS Mercy, out-of-network hospitals with capacity, the VA and other county-designated quarantine sites supporting COVID operations. “It has greatly reduced the load on our staff, increased our surge capacity and availability of our equipment,” Franks says.
All three leaders agree the pandemic has been a defining moment in their careers. “The ‘crisis reveals character’ saying has definitely borne itself out during this,” Handel says.
Editor’s Note: Phil Franks, Matt Wain and Dan Handel all earned Master of Aeronautical Science degrees from Embry-Riddle’s Worldwide Campus.
